Atrial Fibrillation Medical Management
The management of patients with AF should always address three areas: control of the heart rate, stroke risk, and consideration of cardioversion/maintenance of sinus rhythm. Most patients who present with their first episode of atrial fibrillation can be started on oral medications after an initial evaluation with a cardiologist. Patients with prolonged chest pain, congestive heart failure, or a difficult to control heart rate may need to be admitted to the hospital to initiate treatment. Common medications and dosages are shown below:
Control of the Heart Rate
If your heart rate is rapid in AF, your doctor may prescribe medications to slow the bottom chamber of the heart. Three types of drugs can be used to slow the heart rate in AF: these include beta-blockers, calcium channel blockers and digitalis. Common medications and dosages are shown below.
| Medication | Starting Dose | Maximum Dose | Frequency |
|---|---|---|---|
| B-blockers | |||
| Metoprolol | 12.5-25 mg | 200-400 mg | twice daily or once daily (long-acting) |
| Atenolol | 25mg | 200mg | daily |
| Carvedolol | 3.125mg | 25mg | twice daily |
| Ca blockers | |||
| Diltiazem | 30mg | 90mg | three times daily or once daily (long acting) |
| Verapamil | 40mg | 160mg | three times daily or once daily (long acting) |
| Digoxin | 0.125mg | 0.25mg | daily |
Sometimes combinations of the above medications may be required to adequately control the heart rate, for example a β-blocker and digoxin. Your physician may perform a 24-hour heart rate recording or “Holter monitor” to make sure your heart rate is well controlled throughout the day.
Some patients continue to have poor rate control despite multiple medications. Options include consideration of AF ablation (see ablation below) or A-V node ablation and pacemaker placement, which provides complete control of the heart rate without symptoms, but does not correct the underlying AF and renders the patients pacemaker dependent. These options can be discussed with your doctor.
Stroke Risk
The most feared complication of AF is stroke. Anticoagulation can significantly ameliorate this risk. Five large prospective randomized trials comparing warfarin and placebo in patients with nonvalvular AF have been performed that have proven that anticoagulation with warfarin reduces stroke risk in those AF patients at risk , , A pooled analysis performed by the principal investigators of each trial identified four important clinical risk factors for stroke (see Table 3). 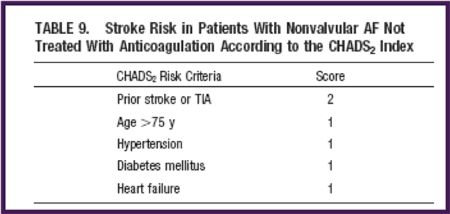 Future epidemiologic studies identified the CHADS2 score as an important determinant of stroke risk in AF. CHADS2 stands for the points given to each risk factor as shown on the chart at the right.
Future epidemiologic studies identified the CHADS2 score as an important determinant of stroke risk in AF. CHADS2 stands for the points given to each risk factor as shown on the chart at the right.
Treatment guidelines for anticoagulation in AF patients, depending on the CHADS2 score, have been published by the American College of Cardiology and American Heart Association and are shown in the table below:
| Score | Risk | Anticoagulation Therapy | Considerations |
|---|---|---|---|
| 0 | Low | None or Aspirin | Aspirin daily |
| 1 | Moderate | Aspirin or Warfarin | Aspirin daily or INR 2.0-3.0 |
| 2 | Moderate or High | Warfarin | INR 2.0-3.0 |
A newer score, the CHADS2-Vasc score has been proposed by the European Society of cardiology and takes into account additional risk factors. The CHADS2-Vasc score is shown below:
CHA2DS2-VASc score for stroke risk in atrial fibrillation
| Feature | Score if present |
|---|---|
| Congestive Heart Failure | 1 |
| Hypertension | 1 |
| Age ≥ 75 years | 2 |
| Age between 65 and 74 years | 1 |
| Stroke/TIA/TE | 2 |
| Vascular disease (previous MI, peripheral arterial disease or aortic plaque) | 1 |
| Diabetes mellitus | 1 |
| Female | 1 |
Anticoagulation guidelines based on the CHADS2-Vasc score are shown below:
| Score | Risk | Anticoagulation Therapy | Considerations |
|---|---|---|---|
| 0 | Low | No antithrombotic therapy (or Aspirin) | No antithrombotic therapy (or Aspirin 75-325mg daily) |
| 1 | Moderate | Oral anticoagulation (or aspirin) | Warfarin INR to 2.0-3.0, or one of the new oral anticoagulation drugs or aspirin 75mg-325mg daily |
| 2 or greater | High | Oral anticoagulation | Warfarin INR to 2.0-3.0, or one of the new oral anticoagulation drugs |
In the past, the only medication available for oral anticoagulation was warfarin. Warfarin is an oral anticoagulant that works by blocking vitamin K production in the liver. Unfortunately there is no standard dose for warfarin, and its effect is measured by a blood test called the INR (international normalized ratio). The warfarin dose must be individualized for each patient and adjusted to maintain the INR between 2.0 and 3.0. Typically blood tests are performed weekly during initiation and eventually reduced to monthly during maintenance. The regular blood tests and dietary restrictions are often an inconvenience to patients. Several newer anticoagulants are being developed that have more predictable effects and do not require blood tests for monitoring. The first of the newer anticoagulants to be approved was a drug named dabigatran (PradaxaTM). A large multicenter randomized trial showed that this drug, when given at the dose of 150ug twice daily, worked as well as warfarin in preventing strokes with less risk of bleeding. Many physicians now consider dabigatran a suitable alternative to warfarin. Side effects include bleeding and an upset stomach. Rivaroxaban (XareltoTM) is another new drug that was recently approved for the prevention of stroke associated with AF. As with dabigatran, a large multicenter study demonstrated that rivaroxaban worked as well as warfarin in preventing stroke with less bleeding. The advantage of riveroxaban is that it only needs to be taken once daily, and no monitoring of blood tests is needed. Another promising new anticoagulant under investigation is a drug called apixaban (EliquisTM) . Currently these drugs are more expensive than warfarin, so you should check with your insurance company if they are covered. All these drugs are also excreted, in part, by the kidneys. So if you have a history of kidney disease you need to discuss with your doctor whether you are eligible to take on of these new drugs. Warfarin, on the other hand, is completely metabolized by the liver, so it can be taken in patients with kidney disease.
All patients with AF due to heart valve disease due to prior rheumatic fever (mitral stenosis), regardless of age, are also at high risk of stroke and should be anticoagulated.
Cardioversion/Maintenance of Sinus Rhythm
Most patients presenting with new onset AF who remain in AF should receive an initial attempt at cardioversion (shock) to restore a normal heart rhythm. Since AF will recur in most patients, the addition of antiarrhythmic agents may also be needed to help maintain sinus rhythm. The decision of when to forgo maintanence of sinus rhythm in favor of anticoagulation and ventricular rate control is a difficult one. In patients with symptoms of palpitations, fatigue, or exertional dyspnea, aggressive attempts to maintain sinus rhythm are certainly warranted. Antiarrhythmic drugs are agents that help the heart maintain a normal rhythm. In general these agents are more potent than the drugs used for heart rate control, and may have additional side effects. These may include fatigue, a slow heart rhythm, and the potential for creating life-threatening heart rhythms in the bottom chambers of the heart. The most potent of these drugs, amiodarone, can also be associated with lung, thyroid and liver toxicities as well as causing problems with vision and nerves. For this reason these drugs are often started in the hospital while the heart rhythm is monitored. Your cardiologist can help decide of a heart rhythm drug is needed and which is best and safest. In the asymptomatic patient, the risk of antiarrhythmic drug therapy must be weighed against the benefit of maintaining sinus rhythm. The commonly used oral antiarrhythmic drugs your doctor may prescribe are outlined in the Table 2 below.
| Drug | Class | Starting dose | Frequency | Total Maximum daily dose | Side-effect |
|---|---|---|---|---|---|
| Quinidine (Quinaglute) | IA | 324 mg | 3x times daily | 1944 mg | Nausea, diarrhea |
| Disopyramide (Norpace) | IA | 150 mg | 4x daily or 2x daily (CR) | 1200 mg | Dry mouth, eyes |
| Flecainide (Tamocor) | IC | 50-100 mg | 2x daily | 400 mg | Metallic taste, fatigue |
| Propafenone (Rhythmol) | IC | 150 mg | 3x daily or 2x daily (SR) | 900 mg | Metallic taste, fatigue |
| Sotalol (Betapace) | III | 80 mg | Twice daily | 320 mg | Slow heart rate, Torsade de pointes VT |
| Dofetilide (Tikosyn) | III | 500 ug | Twice daily | 1000 ug | Torsade de pointes VT |
| Amiodarone (Cordarone) | III | 100-200 mg | Daily | 400 mg | Lung fibrosis, liver failure, hyper/hypothyroidism, neuropathy, optic neuritis |
It should be emphasized that complete suppression of AF with an antiarrhythmic drug is an unrealistic. Even with effective drug therapy, recurrence rates of AF are approximately 50% at 1 year. Often, a more reasonable goal is a reduction in the frequency of AF recurrences. Therefore, each AF recurrence is not necessarily a "failure" of therapy, and drug type or dosage need not be adjusted for infrequent recurrences . This can be discussed with your doctor. The key to successful treatment of AF is tailoring therapy to the individual patient.
Can anticoagulation be stopped after return to sinus rhythm in patients on antiarrhythmic drugs?
Once a patient has been converted to sinus rhythm, the question of stopping anticoagulation always arises. Although it seems intuitively reasonable, there is currently no data to support the assertion that patients in sinus rhythm on antiarrhythmic treatment have a low risk of thromboembolism. Even patients with significant symptoms from AF can have significant asymptomatic episodes. Therefore, in patients treated with antiarrhythmic drugs, the decision to use antiarrhythmic drugs should be independent of the decision to use anticoagulation. Even if apparent sinus rhythm is maintained, anticoagulation should be continued based on the CHADS2 or CHADS2-Vasc score.
