Myocarditis Center
The UCSF Myocarditis Center is a leading center for diagnosis, management, and research on patients with myocarditis. The Myocarditis Center at UCSF closely incorporates advanced cardiovascular specialties, including critical care cardiology, heart failure/transplant and cardiac electrophysiology, to provide comprehensive care for patients with myocarditis and other inflammatory cardiomyopathies.
These clinical efforts are in parallel with research programs that investigate the underlying mechanisms of myocarditis in hopes of better diagnostic and therapeutic strategies for our patients. The UCSF Myocarditis Center was founded on March 20, 2023, as part of the Section of Cardio-Oncology & Immunology by Dr. Javid Moslehi, William Grossman Distinguished Professor in Cardiology. The center includes a team of healthcare providers including physicians, nurses, and clinical coordinators as well as a basic and translational research team. Visit the Moslehi Lab website to read more about the Myocarditis Center's research efforts.
Myocarditis Research at UCSF
UCSF has established a center of excellence dedicated to myocarditis and other inflammatory cardiovascular diseases. Through systematic studies of patients, we collaborate with academic centers and industries to enhance diagnostic and treatment strategies. The ongoing research and collaborative efforts aim to advance our understanding and improve outcomes for patients facing myocarditis and related cardiovascular conditions.
Over the past year, we at UCSF have established an acute myocarditis diagnostic and treatment protocol standardizing approach to patient care.
The UCSF cardio-oncology team has been a pioneer in understanding the cardiac issues of immune checkpoint inhibitors (ICIs) and other immunotherapies. We have both research and clinical areas of focus and have been leading an international effort to understand these toxicities better.
The Moslehi Lab research efforts include establishing mouse models that mimic myocarditis similar to what's observed in ICI-myocarditis. Through these models and innovative approaches, the team seeks to enhance our understanding of interactions between the cardiovascular and immune systems and cancer patients, with the goal of utilizing the immune system to address heart diseases. Find out more about the Moslehi Lab's efforts in myocarditis research.
Clinical areas of focus:
- 1) INFLAME Biorepository is one of our biobanks in which we gather biospecimens from individuals suspected or confirmed to have myocarditis, aiming to enhance our comprehension of the biological attributes of inflammatory heart conditions, including myocarditis, endocarditis, and pericarditis.
- 2) Through the Cardio-Oncology and Immunology Biorepository, we collect biospecimens and through this we want to understand the interconnection between cancer patients and heart disease. We aim to study cancer patients and survivors who either have heart disease or are at risk of developing it.
- UCSF is actively engaged in an international collaboration known as the International ICI-Myocarditis Registry. This initiative involves the gathering of data from patients worldwide who are affected by ICI-Myocarditis. The primary objective of this registry is to gain deeper insights into the unique characteristics of individuals susceptible to this condition.
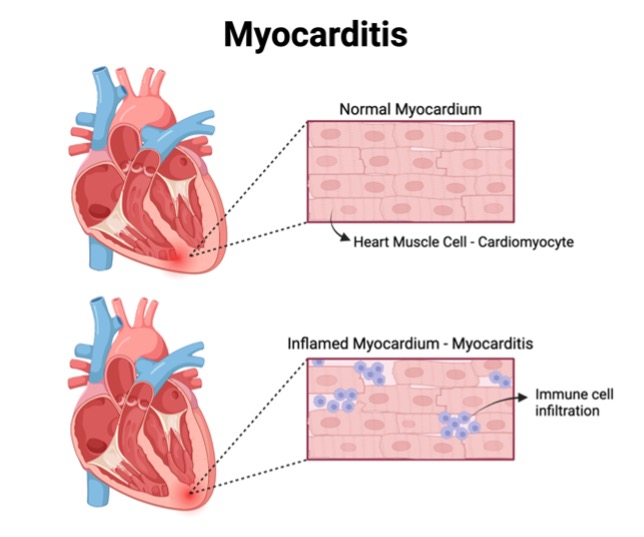
What is Myocarditis?
Myocarditis is inflammation of the heart muscle (myocardium) and can result from various factors such as infections, autoimmunity, and certain drugs, including cancer immunotherapies and vaccines. Common symptoms may include chest pain, shortness of breath, fatigue, heart palpitations, fainting, and leg swelling (edema). Fever at the time of diagnosis or few days before is common. It most commonly affects men between the ages of 30 and 45. However, it can affect people of all ages and sexes.
Types of Myocarditis
Myocarditis can be subclassified, depending on the acuity of symptoms, pathological results (when biopsy has been performed) and possible or probably culprits.
Acute versus Chronic Myocarditis:
Myocarditis can manifest as an acute, critical illness where the symptoms occur suddenly, can be severe and can result in hospitalization. Myocarditis can also be a chronic disease, occurring over months. The distinction between acute and chronic myocarditis lies in the timeframe of symptom onset, with acute cases emerging within a month. Fulminant myocarditis, a severe form of acute myocarditis, is characterized by sudden and intense onset, leading to rapid deterioration.
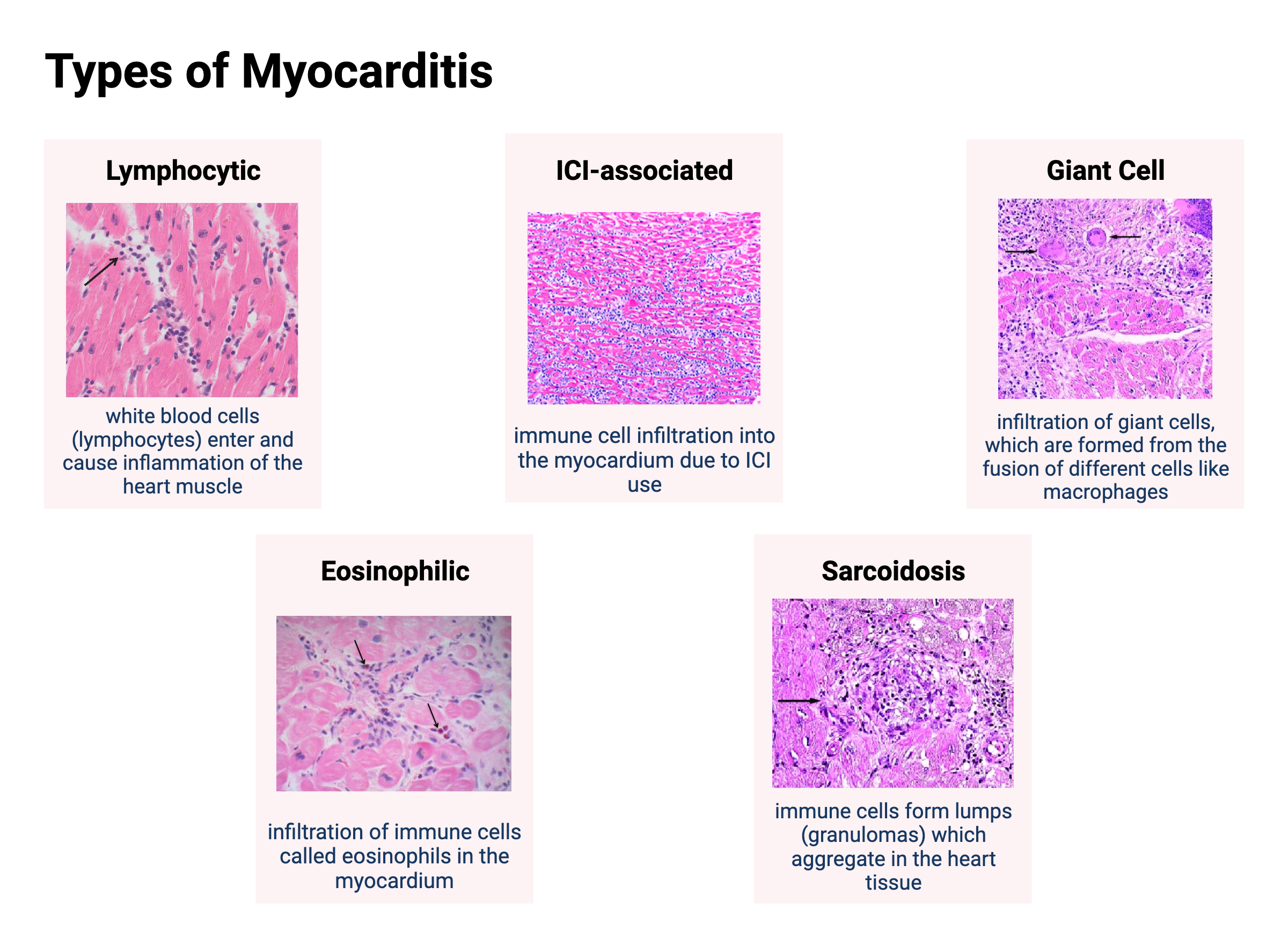
Myocarditis Subgroups Based on Tissue Biopsy
Since myocarditis has traditionally been diagnosed by tissue biopsy, there have been classifications proposed based on the type of inflammation on histology. These include:
- Lymphocytic Myocarditis: This type of myocarditis is distinguished by the infiltration of specific immune cells, called lymphocytes, into the myocardium. It commonly arises from viral infections or immune checkpoint inhibitors (cancer immunotherapies).
- Cardiac Sarcoidosis: Sarcoidosis is characterized by granulomas (clumps of immune cells) on tissue biopsy. Granulomas can be in the heart (leading to cardiac sarcoidosis) or other organs. The accumulation of granulomas in heart tissue disrupts normal function, causing symptoms such as chest pain, shortness of breath, and irregular heart rhythm.
- Giant Cell Myocarditis (GCM): GCM is rare and can be a rapidly progressing form of myocarditis. GCM is characterized by the infiltration of giant cells, formed through the fusion of different immune cells like macrophages. GCM can be severe, causing acute heart failure, cardiogenic shock, and irregular heart rate and rhythm.
- Eosinophilic Myocarditis: Marked by the presence of eosinophils (immune cells) infiltrating the myocardium, this type of myocarditis can result from hypersensitivity reactions to drugs and chemicals, conditions with elevated levels of activated eosinophils in the blood, and certain parasitic infections. Common symptoms include chest pain, shortness of breath, and palpitations.
Causes of Myocarditis
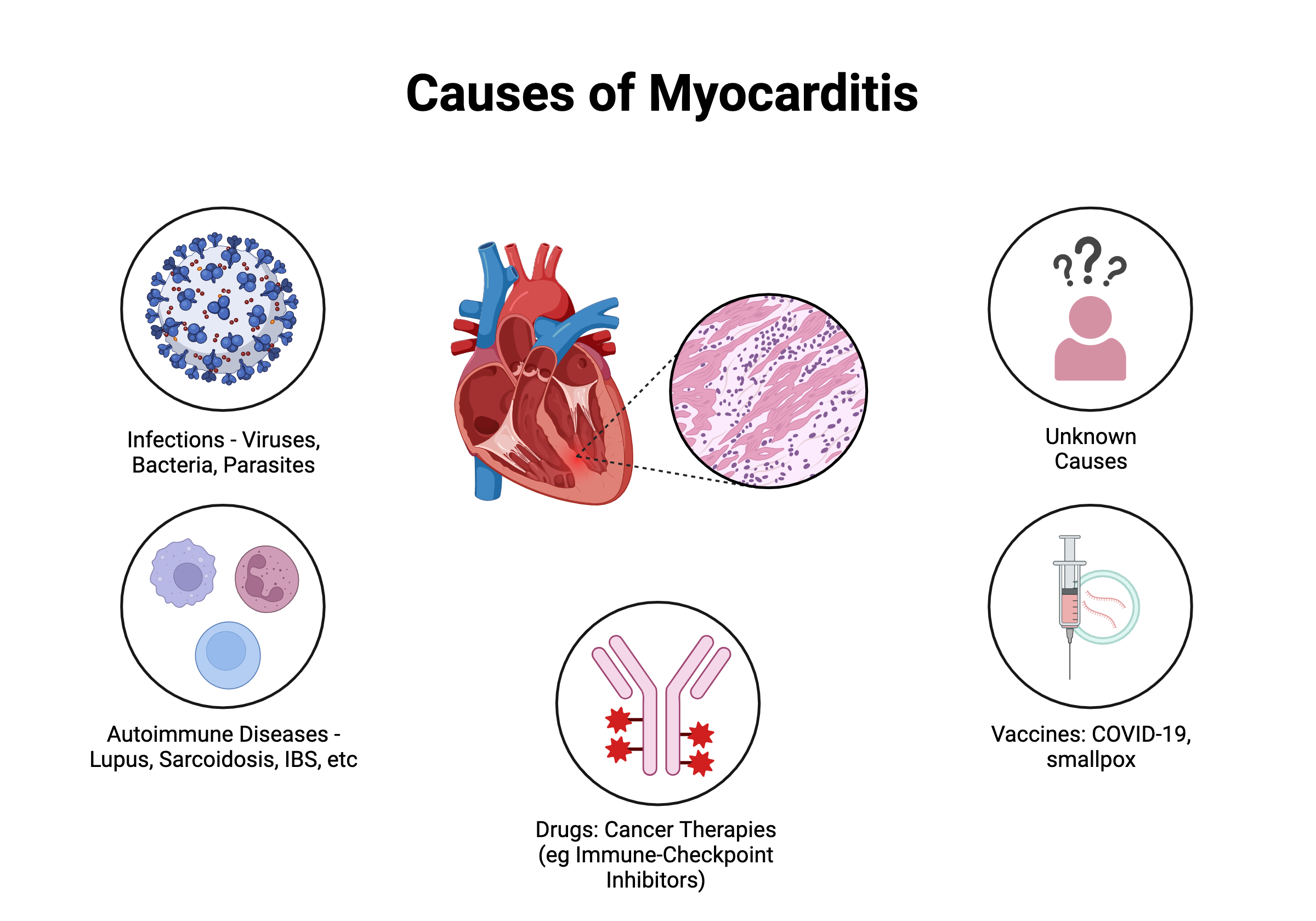
- Viral Infection: Myocarditis, commonly triggered by viral infections, can originate from various sources, including airborne or droplet transmission, as seen with viruses like COVID-19, the common cold (adenovirus), or seasonal flu (influenza). Additionally, gastrointestinal sources, such as enterovirus, blood transmission from hepatitis B and C, parvovirus, or HIV, and insect-borne infections like dengue virus, are also viral causes of myocarditis.
- Other Infections: Myocarditis can also result from infections caused by bacteria, parasites, and fungi. Examples include Lyme disease, a bacterial infection transmitted by ticks, and Chagas disease, a parasitic infection carried by kissing bugs, particularly prevalent in certain regions like South America.
- Systemic Autoimmune Disorders: Conditions characterized by the immune system attacking the body, known as autoimmune disorders, can induce myocarditis when the heart becomes a target. Sarcoidosis, systemic lupus erythematosus, and eosinophilic granulomatosis with polyangiitis are examples of autoimmune disorders linked to myocarditis.
- Drugs: Exposure to certain drugs can lead to myocarditis through either direct cardiotoxic effects or exaggerated immune responses (hypersensitivity). Examples of drugs associated with myocarditis include clozapine, immune checkpoint inhibitors, and cocaine.
- Vaccines: Rarely, vaccinations such as the COVID-19 vaccine and smallpox vaccine have been associated with myocarditis. Although the precise mechanism is unclear, it is thought that vaccines may trigger an immune reaction leading to myocarditis.
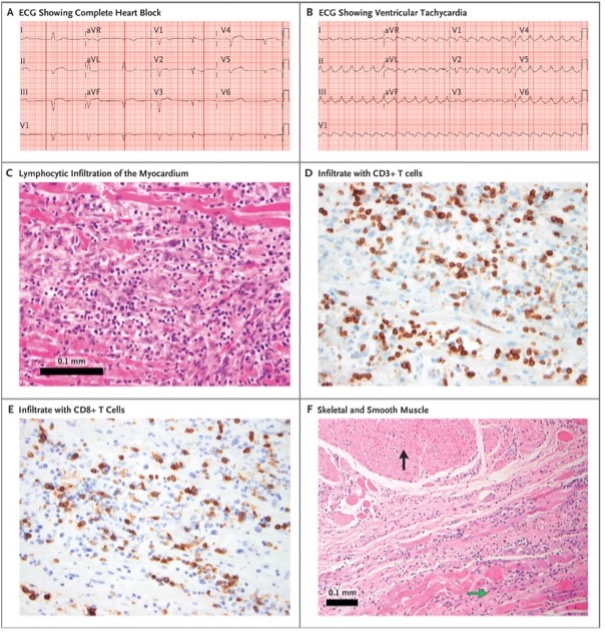
- Immune Checkpoint Inhibitors (ICI): In the last decade, immunotherapies have transformed cancer care. Immune Checkpoint Inhibitors (ICI) unleash the immune cells to fight cancer and have been instrumental in the treatment of previously deadly cancers. Today, up to 50% of cancer patients are eligible for treatment with ICI. ICI, however, can lead to the development of several immune-related adverse events (irAEs) following or during treatment. These irAEs can include acute cardiovascular adverse events, which have also been associated with the treatment of ICI and can include myocarditis, pericarditis, vasculitis, arrhythmias, and cardiac and vascular issues. The UCSF team has been a leader in defining ICI-associated myocarditis.
- Genetic Cardiomyopathies: Recent research has shown that certain gene mutations associated with cardiomyopathy are associated with myocarditis. This works in two ways: first, patients with myocarditis may have genetic mutations that lead to cardiac issues. In addition, patients with genetic cardiomyopathies can be at increased risk of myocarditis. Therefore, at UCSF, all patients with myocarditis are tested for mutations in sarcomeric genes (genes responsible for the basic contraction of the myocardium muscle). Children that develop myocarditis are most likely to have cardiomyopathic genetic mutations.
- Hormonal Effects: It is clear from patient population studies that there are sex differences between the prevalence and severity of myocarditis. Assessing how our hormones (estrogens and testosterone) affect heart inflammation has been a new topic of research.
Diagnosis
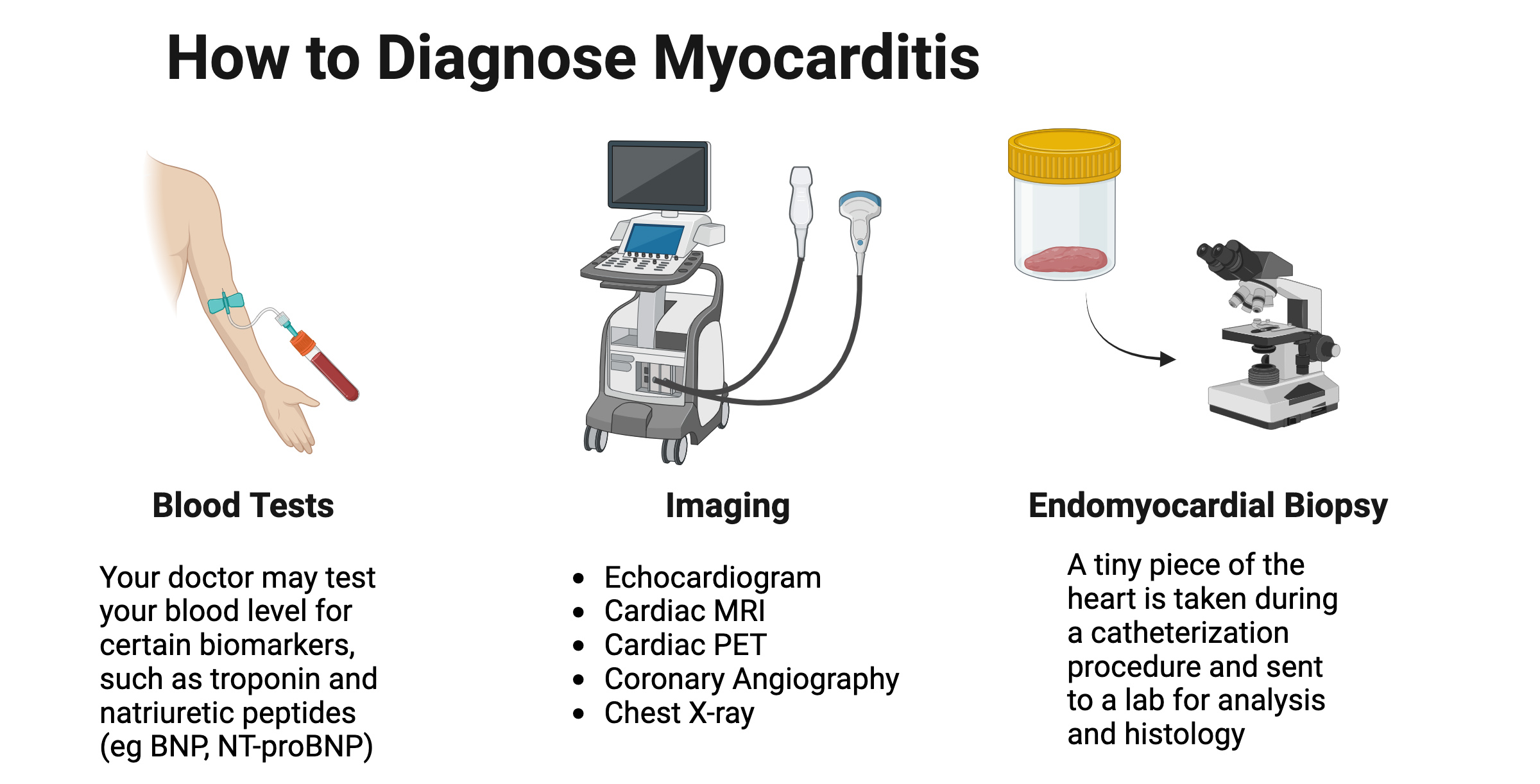
Diagnosing myocarditis can be a complex process, as it involves ruling out other common heart conditions such as heart attack, coronary artery disease (gradual narrowing or complete blockage of vessels supplying blood to the heart), and valvular heart disease (malfunctioning gates between different heart chambers). Your personal medical history is crucial in confirming the diagnosis or providing insights into potential causes of heart inflammation.
To determine the nature of your condition, your healthcare team may employ specialized measures and tests, including:
- Blood Biomarkers: Testing for troponin (indicative of heart injury) and natriuretic peptide (BNP, assessing abnormal increases in heart pressure).
- Echocardiography: A procedure to assess both the function and structure of the heart.
- Left or Right Heart Catheterization with or without Coronary Angiography: These tests evaluate heart function and help rule out vessel blockade or a heart attack.
- Cardiac Magnetic Resonance Imaging: Utilized to identify potential causes of heart disease, confirm inflammation or scarring within the heart, and assess heart function and structure.
- Positron Emission Tomography (PET): Employed to assess the inflammatory condition within the heart.
- Endocardial Biopsy: A biopsy procedure to confirm the underlying causes or inflammation associated with heart disease.
Symptoms
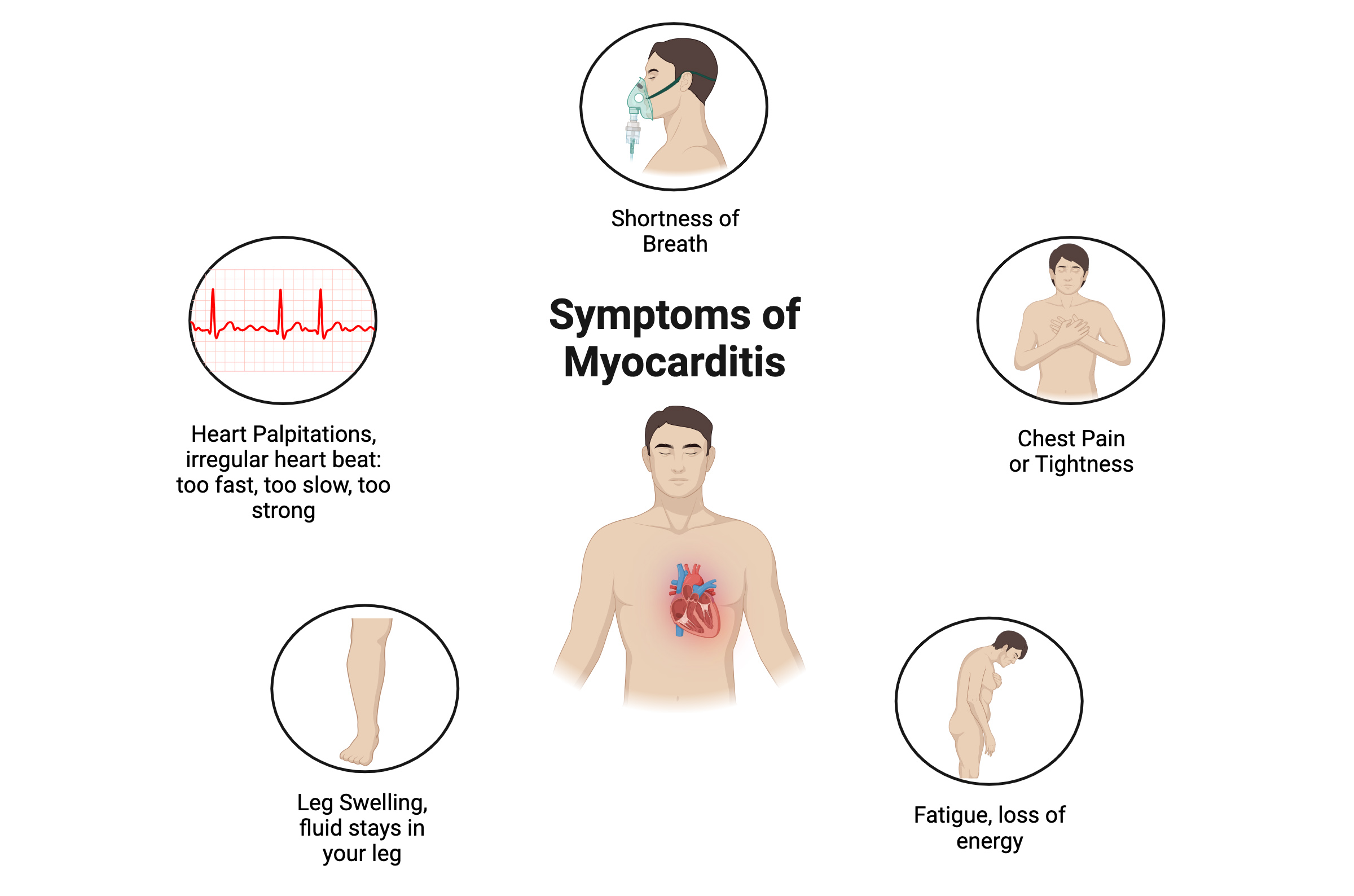
Symptoms of myocarditis vary across patients and causes. During the initial phase of myocarditis, you might experience minimal or no symptoms whatsoever. However, some common symptoms that are often present include:
- Shortness of Breath: When you are out of breath, it might feel like you can't catch enough air or your chest is tight. This feeling can get worse when you're moving around or lying down flat. This feeling can occur at rest or during activity.
- Chest Pain/Tightness: You might feel tightness or squeezing in your chest, whether at rest, active, or lying down. Chest pain may be sharp, spreading to other body parts. If the heart lining is affected, pain may improve when leaning forward and worsen when lying back.
- Fatigue/Loss of Energy: Feeling tired, fatigued, or light-headed like you might faint.
- Leg Swelling: Fluid accumulates in the legs and causes swelling of your legs, ankles, and feet.
- Heart Palpitations: Arrhythmias—having an irregular heartbeat (too fast/slow/strong).
Treatment
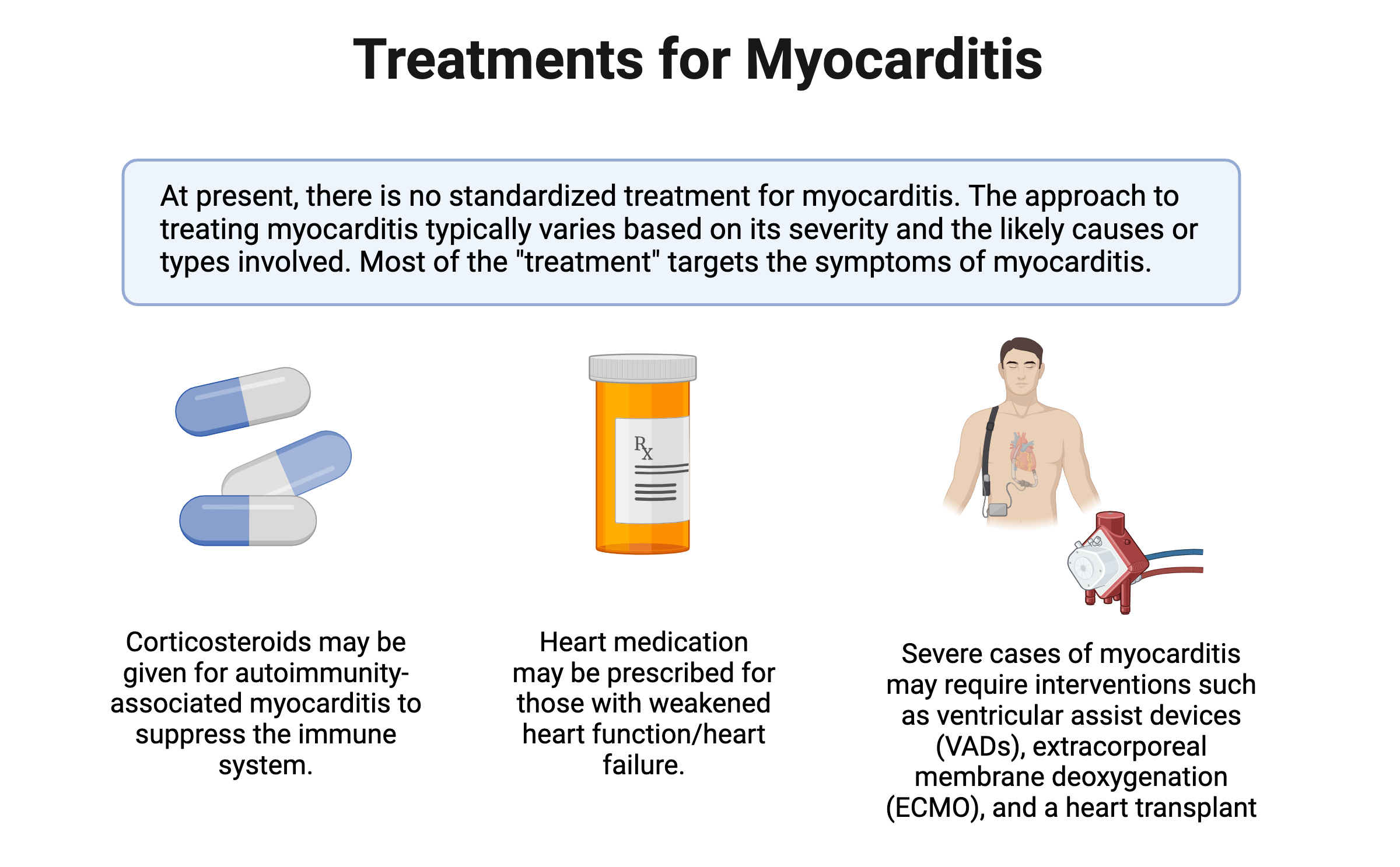
Currently, standardized approach to treating myocarditis does not exist. Interventions are guided by each case’s severity and likely causes. In instances where there is significant heart dysfunction, conventional heart failure medications or devices can be used. When the myocarditis has significant electrical disturbances (arrhythmia or heart block), standard anti-arrythmia medications or devices are often used. For cases associated with autoimmunity, physicians may resort to immunosuppressants, including corticosteroids, to modify the immune response. However, it is crucial to recognize that these immunosuppressive measures provide only temporary control and may not address the underlying myocarditis causes. In severe scenarios, interventions such as ventricular assist devices (VADs), extracorporeal membrane deoxygenation (ECMO), or even a heart transplant may be warranted. The UCSF myocarditis center has recently introduced newer more precision-based therapies for the various types of myocarditis.
References
Amancherla K, Qin J, Wang Y, et al. RNA-Sequencing Reveals a Distinct Transcriptomic Signature for Giant Cell Myocarditis and Identifies Novel Druggable Targets. Circ Res. 2021;129(3):451-453. doi:10.1161/CIRCRESAHA.121.319317
Ammirati E, Bizzi E, Veronese G, et al. Immunomodulating Therapies in Acute Myocarditis and Recurrent/Acute Pericarditis. Front Med (Lausanne). 2022;9:838564. Published 2022 Mar 7. doi:10.3389/fmed.2022.838564
Ammirati E, Moslehi JJ. Diagnosis and Treatment of Acute Myocarditis: A Review. JAMA. 2023;329(13):1098-1113. doi:10.1001/jama.2023.3371
Cooper LT Jr. Myocarditis: Entering the Mainstream. Circulation. 2024;149(9):639-640. doi:10.1161/CIRCULATIONAHA.123.065484
Johnson DB, Balko JM, Compton ML, et al. Fulminant Myocarditis with Combination Immune Checkpoint Blockade. N Engl J Med. 2016;375(18):1749-1755. doi:10.1056/NEJMoa1609214
Lehmann LH, Cautela J, Palaskas N, et al. Clinical Strategy for the Diagnosis and Treatment of Immune Checkpoint Inhibitor-Associated Myocarditis: A Narrative Review. JAMA Cardiol. 2021;6(11):1329-1337. doi:10.1001/jamacardio.2021.2241
Moslehi J, Salem JE. Immune Checkpoint Inhibitor Myocarditis Treatment Strategies and Future Directions. JACC CardioOncol. 2022;4(5):704-707. Published 2022 Dec 20. doi:10.1016/j.jaccao.2022.11.005
Nguyen LS, Cooper LT, Kerneis M, et al. Systematic analysis of drug-associated myocarditis reported in the World Health Organization pharmacovigilance database. Nat Commun. 2022;13(1):25. Published 2022 Jan 10. doi:10.1038/s41467-021-27631-8
Zaha VG, Meijers WC, Moslehi J. Cardio-Immuno-Oncology. Circulation. 2020;141(2):87-89. doi:10.1161/CIRCULATIONAHA.119.042276
